- +34 93 013 08 83
- sale@medicalnanorobots.com
- Autovia de Castelldefels C-31
- Km 190-5 (near Airport)
08820 El Prat de Llobregat (Barcelona)
Why a Modern Surgery System is Essential for Effective Patient Care
In the rapidly evolving landscape of healthcare, the importance of a modern surgery system cannot be overstated. According to the World Health Organization, surgical procedures account for an estimated 11% of the global burden of disease, with over 310 million surgical procedures conducted worldwide each year. As healthcare demands rise, the implementation of advanced surgical systems is essential to improve patient outcomes, streamline operations, and enhance overall efficiency. A well-integrated surgery system not only facilitates better planning and coordination among multidisciplinary teams but also is pivotal in reducing surgical complications and fostering quicker recovery times.
Recent reports emphasize that surgical errors and delays can lead to significant financial burdens on healthcare systems, with studies indicating that up to 60% of surgery-related complications are preventable with optimal procedural approaches. A modern surgery system that leverages cutting-edge technologies, data analytics, and robust training programs can help mitigate these risks. By adopting the latest advancements in surgical techniques and patient management systems, healthcare providers can ensure a higher standard of care, thus benefiting both patients and institutions alike. In essence, the establishment of a modern, efficient surgery system is not merely a luxury—it is a necessity for effective patient care in the contemporary healthcare environment.

Importance of a Modern Surgery System in Healthcare
A modern surgery system is crucial in delivering high-quality healthcare, significantly enhancing patient outcomes. The integration of advanced technologies, minimally invasive techniques, and streamlined processes not only improves surgical precision but also reduces recovery times. This evolution in surgical practices allows for quicker diagnosis and treatment, ensuring that patients can resume their daily lives sooner while minimizing the risk of complications.
Moreover, a contemporary surgical framework fosters interdisciplinary collaboration among healthcare professionals. Surgeons, anesthesiologists, and nursing staff work together seamlessly, utilizing shared information and state-of-the-art equipment to provide comprehensive care. This collaborative environment ensures that the patient's journey is well-coordinated, from pre-operative assessments to post-operative follow-ups.
Ultimately, the importance of a modern surgery system in healthcare cannot be overstated, as it significantly contributes to better patient safety, efficiency, and overall satisfaction in the surgical experience.
Key Components of an Effective Surgery System
An effective surgery system is built on several key components that work in unison to enhance patient care. Firstly, a well-organized pre-operative assessment protocol ensures that each patient is thoroughly evaluated before surgery. This involves detailed medical history reviews, physical exams, and necessary diagnostic tests, which are critical to identifying potential risks. By employing a multidisciplinary team comprising surgeons, anesthesiologists, and nursing staff during this phase, the surgical team can devise tailored plans that prioritize patient safety and optimize surgical outcomes.
Secondly, the surgical environment itself plays a crucial role in the effectiveness of the surgery system. State-of-the-art operating rooms equipped with advanced technology and sterilization methods reduce the risk of infections and complications. The workflow should be streamlined, allowing for swift transitions between surgeries while maintaining a focus on patient safety. Additionally, post-operative care is integral to the system, as it involves monitoring recovery and managing pain effectively. By incorporating follow-up protocols and communication channels for patient support and feedback, healthcare professionals can ensure that patients receive comprehensive care throughout their surgical journey. This holistic approach fosters a culture of safety and quality in surgical practice.
Why a Modern Surgery System is Essential for Effective Patient Care - Key Components of an Effective Surgery System
| Component | Description | Importance |
|---|---|---|
| Preoperative Assessment | Evaluation of patient's medical history and current health status to ensure readiness for surgery. | Reduces risks during surgery and improves outcomes. |
| Surgical Planning | Detailed strategy outlining the surgical procedure, including instruments and techniques to be used. | Ensures smooth execution of surgery and minimizes complications. |
| Anesthesia Management | Administering anesthesia and monitoring vital signs throughout the surgical process. | Crucial for patient comfort and safety during surgery. |
| Intraoperative Monitoring | Continuous observation of the patient’s vital signs and surgical progress during the operation. | Identifies potential issues in real-time for immediate intervention. |
| Postoperative Care | Care given after surgery to monitor recovery and prevent complications. | Essential for confirming successful recovery and addressing any complications swiftly. |
Impact of Technology on Surgical Outcomes
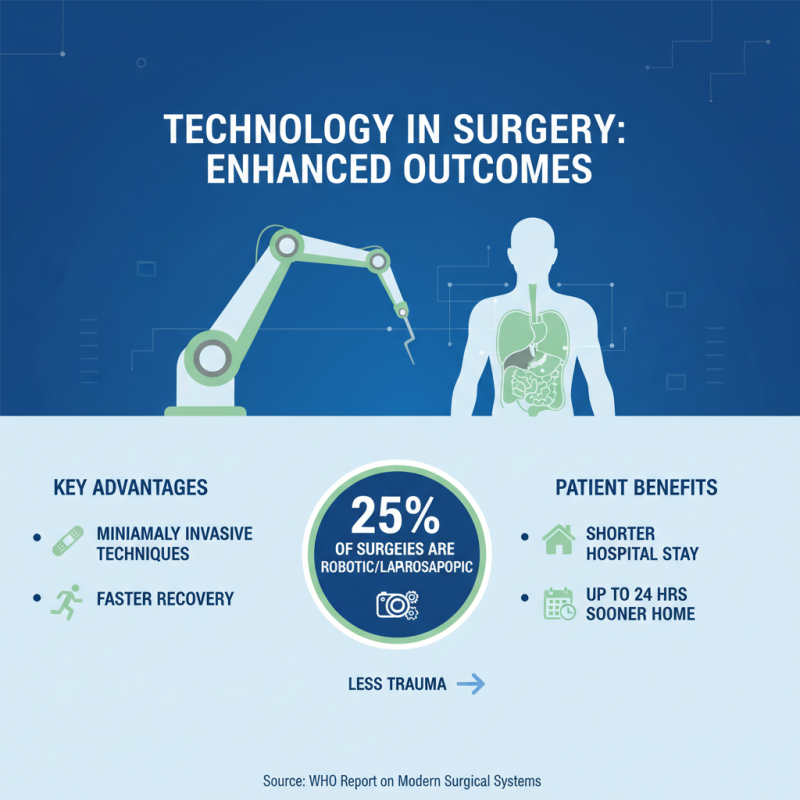
The integration of technology into modern surgical systems significantly enhances surgical outcomes, fundamentally altering the landscape of patient care. According to a report from the World Health Organization, approximately 25% of surgical procedures are performed using minimally invasive techniques, which leverage advanced technologies such as robotic-assisted surgery and laparoscopic instruments. These innovations not only reduce the physical trauma to patients but also lead to shorter recovery times; patients can return home up to 24 hours sooner than those who undergo traditional surgeries.
Furthermore, the utilization of real-time imaging and navigation systems has brought about a paradigm shift in surgical precision. A study published in the Journal of the American College of Surgeons revealed that the adoption of computer-assisted surgical systems led to a 15% decrease in intraoperative complications. This improvement can be attributed to enhanced visualizations and reduced variability in surgical techniques, fostering an environment where surgeons can make more informed decisions during operations. As healthcare continues to advance, the role of technology in shaping better surgical outcomes will only become more pronounced, emphasizing the need for modern surgical systems that integrate these capabilities seamlessly into patient care protocols.
Challenges in Implementing Modern Surgical Systems
Implementing modern surgical systems can significantly enhance patient outcomes, yet several challenges hinder this transition. According to a report by the American College of Surgeons, about 30% of hospitals in the United States lack comprehensive surgical care pathways, which results in variability in patient outcomes. This inconsistency may stem from outdated infrastructure, limited access to advanced technologies, or insufficient training among surgical staff. Moreover, the integration of electronic health records (EHR) into surgical practices remains suboptimal, with studies indicating that less than 50% of surgical teams utilize EHR data to inform decision-making in real time.
Another critical challenge is the financial burden associated with upgrading surgical systems. A recent survey by the Surgical Care Coalition identified that nearly 70% of surgical facilities cite funding as a primary barrier to implementing advanced surgical technologies. Budget constraints often lead to prioritization of urgent care over technological advancements, resulting in missed opportunities to improve surgical efficiency and patient safety. In addition, the rapid pace of technological innovation can overwhelm institutions, especially smaller facilities that may lack the resources for training and adaptation. Addressing these challenges is essential to ensure that modern surgical systems can be effectively integrated into healthcare environments, ultimately leading to superior patient care.
Challenges in Implementing Modern Surgical Systems
Future Trends in Patient Care and Surgical Innovations
The landscape of patient care is undergoing a profound transformation, driven by advancements in surgical innovations that promise to enhance outcomes and improve overall healthcare experiences. One of the most significant trends is the shift towards minimally invasive procedures, which have been shown to reduce recovery times and lower the risk of complications. According to the American College of Surgeons, laparoscopic surgeries can decrease hospitalization duration by up to 50% compared to traditional open surgeries, leading to cost savings for both healthcare systems and patients alike. These innovations not only minimize physical trauma but also contribute to a quicker return to daily activities, thereby boosting patient satisfaction.
Moreover, the integration of technology into surgical practices is revolutionizing patient care. The use of robotic-assisted surgery has expanded rapidly, with a report from Mordor Intelligence indicating a projected growth of the robotic surgery market at a compound annual growth rate (CAGR) of 22.7% from 2021 to 2026. This technological advancement allows for greater precision and flexibility during operations, reducing the likelihood of human error. Additionally, artificial intelligence and machine learning are being employed to analyze patient data, helping surgeons to make more informed decisions pre- and post-operation. As these innovations continue to advance, they are set to redefine standards in surgical practices, ultimately fostering a healthcare environment conducive to improved patient outcomes and safety.
Related Posts
-

Understanding the Surgical Process: Steps, Risks, and Recovery Explained
-

Discovering the Best Surgical Surgeons in 2025: Your Ultimate Guide
-

Best Surgical Systems for Enhanced Precision and Efficiency in 2023
-

Best 10 Advantages of Hybrid Surgery For Modern Medical Practices
-

Top 5 Benefits of Hybrid Surgery: Revolutionizing Surgical Precision and Recovery
-

10 Essential Tips for Choosing the Best Surgery Hospital for Your Needs